CNT-based sensors can be implanted under the skin for a year
Researchers at MIT have built a carbon nanotube sensor that can monitor nitric oxide (NO) in living animals for more than a year. NO is one of the most important signalling molecules in living cells, carrying messages within the brain and coordinating immune system functions. In many cancerous cells, levels are perturbed, but very little is known about how NO behaves in both healthy and cancerous cells.
“Nitric oxide has contradictory roles in cancer progression, and we need new tools in order to better understand it,” says Michael Strano, the Carbon P. Dubbs Professor of Chemical Engineering at MIT. “Our work provides a new tool for measuring this important molecule, and potentially others, in the body itself and in real time.”
The sensors can be implanted under the skin and used to monitor inflammation - a process that produces NO. This is the first demonstration that nanosensors could be used within the body for this extended period of time. Such sensors, made of carbon nanotubes, could also be adapted to detect other molecules, including glucose. Strano’s team is now working on sensors that could be implanted under the skin of diabetic patients to monitor their glucose or insulin levels, eliminating the need to take blood samples.
Carbon nanotubes - hollow, one-nanometre-thick cylinders made of pure carbon - have drawn great interest as sensors. Strano’s lab has recently developed carbon nanotube sensors for a variety of molecules, including hydrogen peroxide and toxic agents such as the nerve gas sarin. Such sensors take advantage of carbon nanotubes’ natural fluorescence, by coupling them to a molecule that binds to a specific target. When the target is bound, the tubes’ fluorescence brightens or dims.
Strano’s lab has previously shown that carbon nanotubes can detect NO if the tubes are wrapped in DNA with a particular sequence. In the new paper, the researchers modified the nanotubes to create two different types of sensors: one that can be injected into the bloodstream for short-term monitoring and another that is embedded in a gel so it can be implanted long-term under the skin.
To make the particles injectable, Iverson attached PEG, a biocompatible polymer that inhibits particle-clumping in the bloodstream. She found that when injected into mice, the particles can flow through the lungs and heart without causing any damage. Most of the particles accumulate in the liver, where they can be used to monitor NO associated with inflammation.
“So far we have only looked at the liver, but we do see that it stays in the bloodstream and goes to kidneys. Potentially, we could study all different areas of the body with this injectable nanoparticle,” Iverson says.
The longer-term sensor consists of nanotubes embedded in a gel made from alginate, a polymer found in algae. Once this gel is implanted under the skin of the mice, it stays in place and remains functional for 400 days; the researchers believe it could last even longer. This kind of sensor could be used to monitor cancer or other inflammatory diseases, or to detect immune reactions in patients with artificial hips or other implanted devices, according to the researchers.
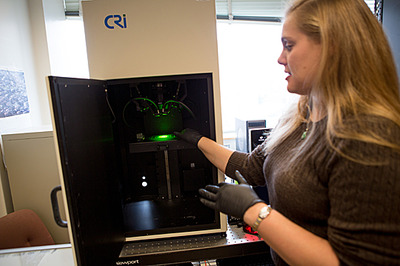
Once the sensors are in the body, the researchers shine a near-infrared laser on them, producing a near-infrared fluorescent signal that can be read using an instrument that can tell the difference between nanotubes and other background fluorescence.
Iverson is now working on adapting the technology to detect glucose, by wrapping different kinds of molecules around the nanotubes. Most diabetic patients must prick their fingers several times a day to take blood glucose readings. While there are electrochemical glucose sensors available that can be attached to the skin, those sensors last only a week at most, and there is a risk of infection because the electrode pierces the skin.
Furthermore, Strano says, the electrochemical sensor technology is not accurate enough to be incorporated into the kind of closed-loop monitoring system that scientists are now working towards. This type of system would consist of a sensor that offers real-time glucose monitoring, connected to an insulin pump that would deliver insulin when needed, with no need for finger pricking or insulin injection by the patient.
“The current thinking is that every part of the closed-loop system is in place except for an accurate and stable sensor. There is considerable opportunity to improve upon devices that are now on the market so that a complete system can be realised,” Strano says.
Ultra-thin fibre microphone monitors power grid systems
Immune to extreme heat and high voltage, the new device could listen for problems inside...
AI-powered wearable turns gestures into robot commands
A new wearable system uses stretchable electronics and artificial intelligence to interpret human...
Graphene-based solar cells power temperature sensors
Researchers have demonstrated the ultra-low-power temperature sensors powered by graphene-based...




